Laser refractive surgery with the excimer laser has revolutionized the field of vision correction. While many of these procedures have focused on cosmetic outcomes, allowing patients to become spectacle-free, excimer laser refractive surgery also offers substantial therapeutic benefits for individuals with corneal irregularities. This article delves into the concept of total corneal wavefront analysis and its pivotal role in enhancing therapeutic excimer laser refractive surgery results, particularly for patients with irregular corneas.
Historical Perspective
Traditionally, our approach to corneal wavefront analysis relied on topography-based corneal wavefront data obtained from instruments like Scheimpflug and Placido systems, which combine technologies to image the cornea’s surface. Additionally, we conducted total ocular wavefront analysis with a pyramidal image system, evaluating the wavefront of the entire eye. Both approaches played a significant role in planning refractive surgeries (Figure 1). However, these methods primarily focused on anterior corneal data or encompassed the entire eye, leaving room for further improvement.
Total Corneal Wavefront Analysis
The introduction of total corneal wavefront analysis signifies a substantial leap forward in our ability to assess and plan therapeutic excimer laser refractive surgeries. This innovative approach, made possible by integrating various technologies, enables the comprehensive evaluation of the entire cornea, including both its anterior and posterior surfaces. It combines Placido disk corneal topography and high-resolution OCT-based anterior segment tomography (MS-39 system) to provide a complete analysis of the total corneal wavefront (Figure 1).

The Importance of Posterior Corneal Surface
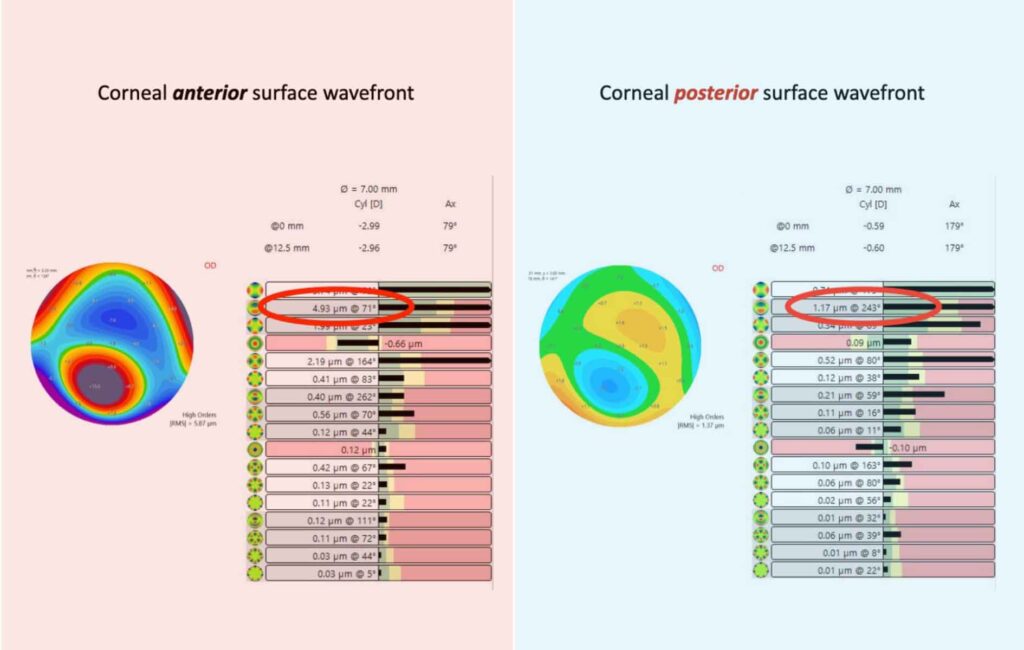
One critical aspect of total corneal wavefront analysis is the consideration of the posterior corneal surface. This component is often overlooked in traditional wavefront analysis, but its impact on the eye’s overall optical quality can be profound. The posterior corneal surface, in conjunction with the lens and other internal factors, significantly contributes to high-order aberrations (Figure 2). By accounting for these posterior corneal aberrations, we can achieve more precise and tailored ablation profiles in many cases.
Clinical Applications
Total corneal wavefront analysis proves particularly valuable in cases involving irregular corneas, such as those with keratoconus or post-surgical irregularities. For these patients, the primary goal is therapeutic, with the aim of improving visual function and alleviating corneal disorders. Minimizing ablation profiles is a priority to avoid exacerbating inflammation and potential haze. Total corneal wavefront analysis provides the necessary data to fine-tune the ablation, addressing both high and low-order aberrations before or after excimer laser surgery.
Combined Therapies
Integrating total corneal wavefront analysis with this approach offers a comprehensive therapeutic solution for irregularities. However, in some instances, excimer laser surgery alone may not be sufficient for irregular corneas. PACE (PTK-Assisted Customized Epi-on) cross-linking, which flattens the cornea without tissue removal, can be an excellent adjunctive treatment. Femtosecond-assisted Corneal Allogenic Intrastromal Ring Segments (femto-CAIRS) implantations are also a promising option as an adjunctive treatment in such cases.
Conclusion
Total corneal wavefront analysis, facilitated by the MS-39 system, represents a significant advancement in therapeutic excimer laser refractive surgery. It enables comprehensive assessment and planning, particularly in cases of irregular corneas. By considering both anterior and posterior corneal surfaces, we can tailor ablation profiles to optimize therapeutic outcomes while minimizing tissue removal. This approach expands our options for therapeutic excimer surgery, emphasizing the importance of improving both visual acuity and the quality of vision in patients with irregular corneas.
You can read the coverage of the talk on this topic by ELZA’s corneal surgeon, Dr. Dr. Emilio Torres-Netto, MD, PhD, FWCRS, here.