Wavefront-guided transPRK is a precise tool for fine-tuning the irregularities of keratoconus. It’s not intended for advanced cases but rather for those requiring less adjustments to achieve a better corneal shape and an increase in vision with glasses.
Wavefront-guided transPRK is a precise tool for fine-tuning the irregularities of keratoconus. It’s not intended for advanced cases but rather for those requiring less adjustments to achieve a better corneal shape and an increase in vision with glasses.
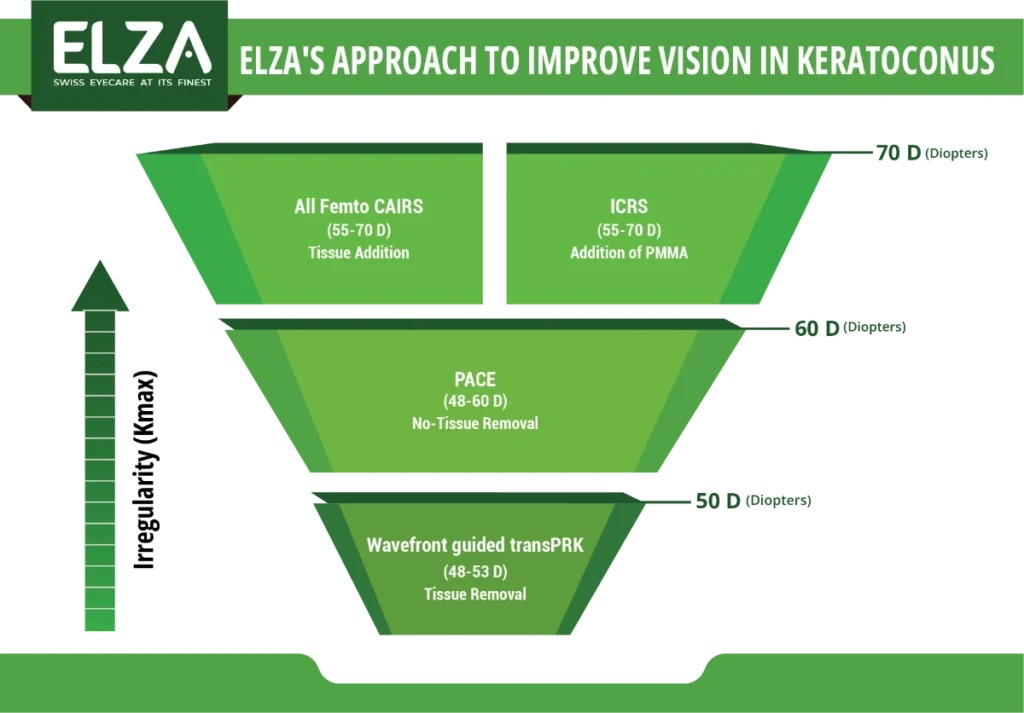
The ELZA pyramid illustrates when we consider using the excimer laser in treatment: while other methods like Femto-CAIRS, ICRS, and ELZA-PACE provide a stronger flattening effect, they are “unspecific,” meaning the amount of flattening they achieve is less predictable. This is why we use Femto-CAIRS, ICRS, and ELZA-PACE first in highly irregular corneas.
Interestingly, these procedures can be combined—a cornea regularized with ELZA-PACE can be further refined using wavefront-guided transPRK.
Unlike ELZA-PACE, wavefront-guided transPRK requires the removal of small amounts of stromal tissue. Since the stroma forms the structural foundation of the cornea and is naturally thinner and more fragile in patients with keratoconus or other corneal ectasias, this procedure must be reserved for corneas that are biomechanically strong enough.
To ensure stability, the cornea must first be cross-linked (either with a standard CXL procedure or ELZA-PACE customized cross-linking). After the corneal shape has stabilized—usually a process that takes up to 12 months—we can then evaluate whether the cornea is suitable for lasering. A comprehensive assessment of the cornea’s shape and biomechanical strength will help determine if it’s safe to proceed.
In some cases, CXL and wavefront-guided transPRK can even be combined for effective treatment.
Wavefront-guided PRK for keratoconus can significantly enhance patients’ visual quality. The excimer laser platform used by ELZA, the SCHWIND AMARIS, stands out for its unique ability to selectively correct higher-order wavefront errors (HOAs). These HOAs occur because the cone in keratoconus creates increasing irregularities in the corneal surface.
Higher-order aberrations (HOAs), uncorrectable with glasses, cause visual disturbances in keratoconus, including ghosting, blurring, double or triple vision, and glare or starbursts at night. Wavefront-guided transPRK targets these aberrations, minimizing laser tissue removal and significantly enhancing visual quality.
We opt for laser treatment only after cross-linking. The rationale behind this approach is that, despite the high success rate of cross-linking, it does not guarantee 100% efficacy: in 3 to 7% of cases, keratoconus may still progress even after comprehensive cross-linking. Additionally, though exceedingly rare (0.5%), some corneas may undergo significant flattening post-cross-linking. Therefore, the safest approach is to delay laser procedures until the corneas have stabilized.
Until recently, a critical piece of information was missing for accurately lasering a cornea post-cross-linking: the exact amount of corneal tissue removed by an excimer laser pulse following CXL.
Is it the same amount as in a non-cross-linked cornea? Or 20% less? Perhaps 40% more? Lacking knowledge of the precise ablation rate leads to inaccuracy in results.
Our group conducted an extensive study to determine the ablation rate in corneas post-CXL, with findings published in the American “Journal of Refractive Surgery”: https://pubmed.ncbi.nlm.nih.gov/25250420/
We discovered that in a cornea treated with CXL, each excimer laser pulse removes 12% less tissue compared to a cornea without CXL. This insight significantly enhances the precision of our treatments.
Here’s a comparison of visual acuity and simulated vision (based on corneal wavefront analysis) before and after the wavefront-guided transPRK treatment. After the treatment, issues like double vision and halos improve, and the sharpness and contrast of what you see gets better. If the patient wears glasses, their prescription might change or even become stronger . The primary goal is to improve vision and contrast.
Beyond the improvement in visual acuity, it is primarily the enhancement in image quality that benefits our patients. Unlike visual acuity, “image quality” as a concept lacks a simple metric in ophthalmology.
Thus, improving visual acuity is just one aspect of the overall enhancement. Equally crucial is that an increase in visual acuity by over 50% can augment three-dimensional vision (depth perception), offering a comprehensive improvement in visual experience.










Get in touch
During office hours.
Email us.
Make an appointment, and come to see us.
Thank you for writing a review on google.
Contact us here, we will get in touch with you.
Zoom online consultation for our international patients.
Contact us here, we will get in touch with you.
Contact us here, we will get in touch with you.
Stay informed & get the newsletter
You have successfully joined our subscriber list.
Newsletter abonnieren & informiert bleiben
Sie haben sich erfolgreich in unsere Abonnentenliste eingetragen.
Bitte bestätigen Sie Ihr Abonnement, indem Sie auf den Link in der E-Mail klicken, die wir Ihnen gerade geschickt haben.