A recently published article in Ophthalmologische Nachrichten reviewed the current state of corneal cross-linking (CXL) in patients with progressive keratoconus and thin or ultra-thin corneas—a group historically excluded from standard treatment protocols. The review, authored by ELZA’s medical director, Prof. Farhad Hafezi, MD, PhD, FARVO, addresses a long-standing clinical challenge: how to safely stabilize ectatic progression when stromal thickness falls below the conventional 400 µm threshold required by the Dresden protocol.
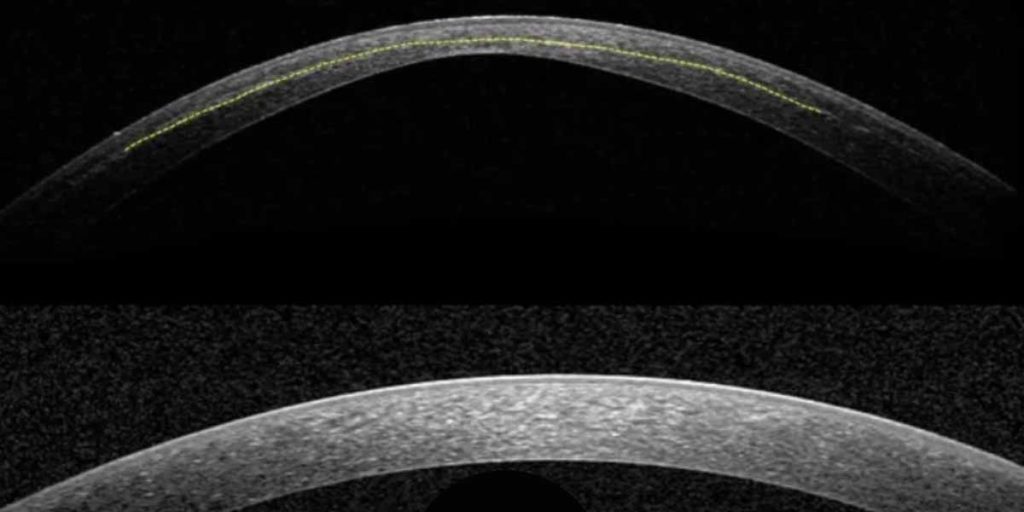
Standard epithelium-off CXL relies on maintaining a non-cross-linked posterior stromal safety margin of approximately 70 µm to protect the corneal endothelium from UV-A exposure. This requirement has traditionally limited treatment options for advanced keratoconus, often leaving keratoplasty as the only remaining intervention. Over the past decade, several techniques have attempted to extend CXL eligibility to thinner corneas, including stromal swelling with hypo-osmolar riboflavin, contact lens–assisted CXL, and approaches preserving epithelial islands over the thinnest regions.
The Ophthalmologische Nachrichten article critically reviews these methods and highlights their limitations, including unpredictable pachymetric changes, reduced oxygen availability, and less consistent biomechanical stiffening. A key conceptual shift discussed in the review is the move away from modifying the cornea to fit the technique, toward adapting the CXL protocol itself to individual corneal properties.
Central to this approach is individualized cross-linking using the sub400 protocol. Rather than enforcing a fixed minimum thickness, the protocol adjusts UV-A irradiation time based on stromal thickness while maintaining standard irradiation intensity. This algorithmic strategy models the interaction between UV-A energy, riboflavin absorption, and oxygen diffusion, allowing cross-linking to be confined to the anterior stroma while preserving an endothelial safety margin.
Clinical data summarized in the review report high rates of tomographic stability in thin and ultra-thin corneas, including eyes with stromal thicknesses well below 400 µm. Follow-up data extending to two years show sustained stabilization without evidence of endothelial decompensation, and a correlation between irradiation time and demarcation line depth supports the predictability of this individualized approach.
From a clinical standpoint, the review underscores the relevance of personalized CXL strategies for patients with advanced disease, particularly younger individuals at risk of rapid progression. By expanding eligibility for biomechanical stabilization, individualized protocols may reduce the need for corneal transplantation in selected cases.
At the ELZA Institute, these concepts are applied within a structured, evidence-based framework for keratoconus management. The Ophthalmologische Nachrichten review reflects the broader trend toward protocol personalization in corneal cross-linking, emphasizing safety, transparency, and alignment with established photochemical principles.