Highlights from ESCRS 2025 ELZA Institute Sunday sessions in Copenhagen, featuring advances in keratoconus, glaucoma, and corneal surgery
Since 2009, ELZA’s surgeons and researchers have been leading advances in corneal cross-linking (CXL) for thin corneas.
Thin (<400 µm) and ultra-thin (≤220 µm) corneas have long presented a treatment challenge because of minimum thickness safety limits intended to protect the corneal endothelium from ultraviolet (UV) damage. The original “Dresden protocol” excluded corneas thinner than 400 µm to safeguard these endothelial cells, which are essential for nourishing the cornea and maintaining its transparency by regulating hydration. Importantly, these cells do not regenerate once damaged by UV exposure. At the time the Dresden protocol was developed, a 70 µm uncross-linked stromal safety margin was calculated as necessary to prevent UV-induced endothelial injury.
Our pioneering research has led to innovative protocols that safely and effectively treat corneas well below this 400 µm threshold, culminating in the current state-of-the-art ELZA-sub400 protocol.
Keratoconus – and related corneal ectasias, including post-LASIK ectasia – cause progressive thinning. In the past, if detected late, cornea that had thined to less than 400 µm were excluded from receiving Dresden protocol CXL.
The optical coherence tomography image below illustrates this challenge: two corneas are shown: one 220 µm thick (top) and one 420 µm thick (bottom). Only the thicker cornea could be cross-linked, despite the thinner one requiring treatment the most.
In 2009, Prof. Hafezi and colleagues introduced hypoosmolar riboflavin, which transiently swells thin corneas to a safer thickness, allowing CXL without risking endothelial damage. Although this approach was widely adopted, this method’s variability in corneal swelling response poses challenges: insufficient swelling in some patients means that the treatment cannot go ahead.
Other thin cornea CXL protocols have been developed, such as contact lens–assisted CXL, where a riboflavin-soaked contact lens is placed on the cornea to artificially increase its thickness during UV irradiation. However, this method produces less biomechanical strengthening than hypoosmolar riboflavin, because, as explained below, the contact lens acts as a barrier that reduces oxygen diffusion into the cornea.
CXL relies on a photochemical reaction. In epi-off CXL, the corneal epithelium is removed so riboflavin (vitamin B2) saturates the stroma, the cornea’s main structural layer. UV energy then activates riboflavin and stromal oxygen, generating reactive oxygen species (ROS) that induce cross-links between collagen fibrils, strengthening the cornea. Oxygen is rate-limiting, influencing cross-linking depth and efficacy. Understanding and modelling these reagent interactions has formed the foundation of modern thin cornea CXL approaches. ELZA and collaborator Dr. Sabine Kling published this modelling algorithm in 2017.
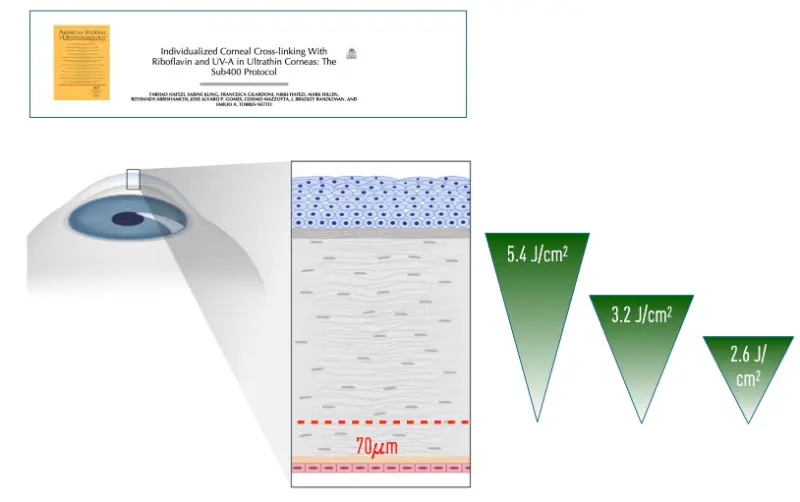
By modelling the entire photochemical reaction, we quantify how much cross-linking a given UV energy dose achieves. Thus, UV fluence can be adjusted by altering exposure duration. Measuring corneal thickness at its thinnest point allows tailoring UV irradiation time to maximize cross-linking while maintaining a minimum 70 µm safety margin of uncross-linked, riboflavin-saturated stroma above the endothelium – optimizing efficacy and safety.
The sub400 protocol achieves cross-linking depths customized to corneal thickness, often less than the ~330 µm effect in thicker corneas treated with the Dresden protocol. This tailored fluence minimizes endothelial UV exposure while ensuring biomechanical strengthening. Clinical studies at ELZA report a 90% success rate in halting progression in corneas as thin as 214 µm, with no endothelial damage or decompensation.
Discover how ELZA’s scientific rigor and clinical expertise continue to redefine safety and effectiveness standards in thin cornea cross-linking.
Get in touch
During office hours.
Email us.
Make an appointment, and come to see us.
Thank you for writing a review on google.
Contact us here, we will get in touch with you.
Zoom online consultation for our international patients.
Contact us here, we will get in touch with you.
Contact us here, we will get in touch with you.
Stay informed & get the newsletter
You have successfully joined our subscriber list.
Newsletter abonnieren & informiert bleiben
Sie haben sich erfolgreich in unsere Abonnentenliste eingetragen.
Bitte bestätigen Sie Ihr Abonnement, indem Sie auf den Link in der E-Mail klicken, die wir Ihnen gerade geschickt haben.